Inorganic Phosphate
A Syndromic Approach: Respiratory Alkalosis & Hypophosphatemia
LTCOVID.com
Thanks for visiting!
To translate this page, select your
language from the dropdown menu below:
Syndromes in Medicine are named illnesses that typically group together several symptoms or findings.
Initially, these findings are frequently overlooked as a cluster that goes together, defining a single disease process. The link isn't made until someone makes it. Recognizing a specific syndrome is most useful when it announces possible health problems that commonly, would not be sought after. Syndromes often get weird names assigned to them, or the names of their discoverer(s). Again, what is important is knowing that a syndromic patient is perhaps prone to other illnesses associated with a given syndrome.
Here's one example: Tricho-Rhino-Phalangeal (TRP) Syndrome.
This happens in young children. They manifest with thin hair (tricho), a bulbous pear-shaped nose (rhino) and an X-ray of their hand (when they are age 9 or less) which shows "coning" of the epiphyseal growth plate (phalangeal). What does recognizing the syndrome help us to do? These children frequently get pneumonia, often bilateral. These children often get hip problems (aseptic necrosis). They can get other health problems such as dental problems as well.
But the point here is that certain findings that don't intuitively fall together, do in fact, fall together.
Many syndromes, such as TRP, commonly display a certain pattern of inheritance. It is a pretty rare disorder, inherited as an autosomal dominant with incomplete penetrance. Unimportant for our purpose here.
But syndromic findings also occur in non-genetic illnesses that do not transmit from parent to offspring.
Does our "long-term" COVID-19 questionnaire help us to identify findings that should be grouped together to better understand this variant of COVID-19?
"Breathing differently"
In what follows, the responses to the questionnaire are the only source of information.
That means we do not have results from the laboratory or other tests.
The the information that we do have from these responses, linked to what is already known in Medicine, allows us to group certain findings together.
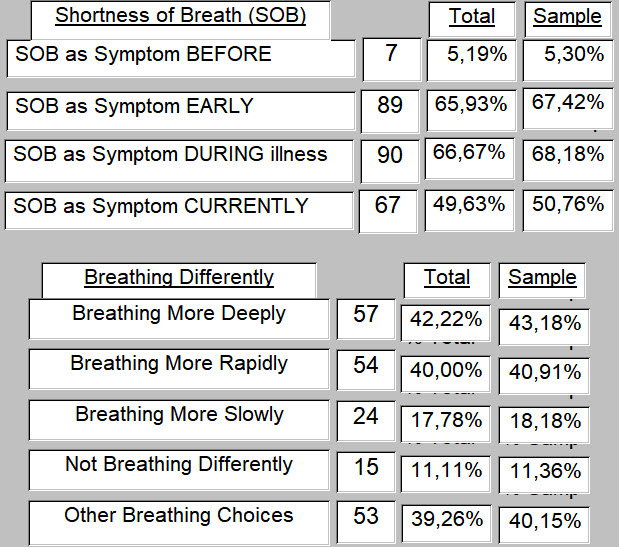
Only 15 respondents indicated that they are not breathing any differently.
117 said that they were.
57 are breathing more deeply, 54 more rapidly and 20 (not shown below) responded that they are breathing both more deeply and more rapidly.
So this begins to evoke the classic findings of hyperventilation. Not for all, but perhaps some.
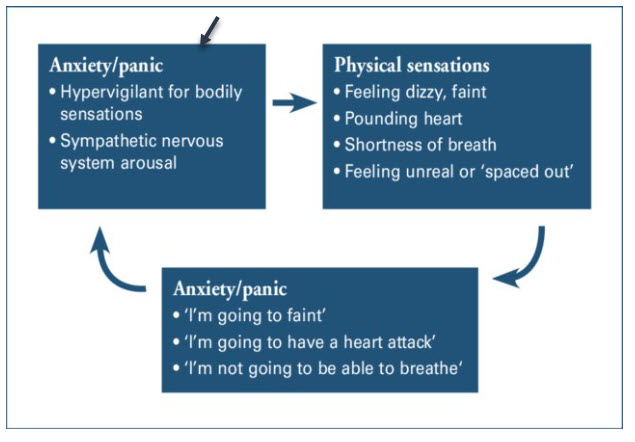
Hyperventilation is common in anxiety states.
77 (58.33%) indicated that they experience Anxiety. 44 (33.33%), Panic, and 72 (54.55%), Fearfulness.
79 (59.8%) are More Attuned to Bodily Changes. 25 (26.5%) said Perhaps, and those two together = 114 or 86.4%, with 21(15.9%) saying that they are not more attuned to bodily changes.
Sometimes, for instance when one is having a symptomatic heart attack or an asthma attack, noticing one's symptoms can lead to anxiety, fearfulness and even panic. A silly thing to say?
Am I starting here to work towards an argument that this "long-term" variant of COVID-19 is just an illness that is "all in their minds"? No. Not at all.
Another observation.
A typical day for many (our Q. 30), includes making measurements of pulse and peripheral oxygen saturation (spO2). This is presumeably with a home pulse oximeter. And 61 (45.19%) do this daily (or more often).
A choice available in the same question is: "measuring my end-tidal CO2."
No one selected this. Not one.
That lack of response is not surprising. Capnography (measuring end-tidal CO2) is not readily available, and the equipment is typically significantly more expensive than a pulse oximeter.
What's the point?
Well, without a measurement to say that expired CO2 levels were abnormally low in these respondents, arguing the presence of hyperventilation lacks a critical test result.
And yet on a clinical basis (reported subjectively by the respondents) it would appear to be present not infrequently.
Time for an Anecdote
Before going to Medical School, I worked in the ER at the George Washington University Medical Center.
It's also where I trained subsequently, and where my two children were born. Like many things and people that have become old, that large hospitalit has been swept away. I recall in particular in my mind's eye, the steps at the south end of the hospital. They were stone, and had been worn concave by the passing of gillions of shoes. Medical students running for lab results. Interns and Residents running to make Rounds or get to the OR on time. Even patients in a hurry to get out of there and go home. And many other pairs of shoes as well. Waiting for an elevator often added nothing but more delay and uncertainty. We all took the stairs. And we wore them away. And each step seemed to remind to just hurry, and get it done. Whatever "it" was on that day.
So when before Medical School I was a Nursing Assistant, I had many duties. One such duty was to make sure that I had maintained an adequate stock of brown paper bags. When out of stock, I would push a cart through the halls and elevators (couldn't do the stairs with the cart), and obtain them from Mr. Lanada at Central Service Supply, in the basement. Mr. Lanada in shirt and tie, 5 or 6 kind and patient women in scrubs and hats. Always calm in Central Service. Not like the ER.
Not infrequently, when a patient presented to our Emergency Room with symptoms that a Nurse and Physician (not me) had decided represented a panic or anxiety attack, I was often called upon yet again to administer the cure. They would add the title "Doctor" to my first name as they called me to say that I had "a brown bag patient" in one of the ER's exam rooms. Yes, the patient had usually been placed in the "Psych Room."
I would go in, introduce myself, and explain that we were going to work together to bring this attack to an end. At that time (1974) patients seemed less interested in knowing what Google and the Internet had to say about my proposed therapeutic intervention, and I calmly and systematically explained the proposed process before beginning the intervention.
I would roll up the edges of a brown paper bag, and place the opening over the patient's nose and mouth, doing this gently and reassuringly: Getting a good fit like when one puts on a surgical mask these days to go anywhere.
Brown paper bag, firmly held in place with my two hands.
Most patients mentioned through the bag that they couldn't breathe. I reassured them, and made sure the edges of the bag were nicely sealed against the face. The first few breaths were usually very large: bag quite full ... bag quite empty. Made a crinkly paper sound. Sometimes so large that the bag would tear and I had to get its replacement. No supplemental oxygen was applied during most treatments, but I guess now, it could have been. Never seemed to be necessary. Through the bag, many patients mentioned that they were going to faint. Or that they were going to have a heart attack. And as they pronounced these words, they did not seem at all to be joking.
After 3 to 5 minutes, tingling in the patient's fingers and toes typically began to diminish. As did the frequency and depth of respiration. Within an additional 10 to 15 minutes, all the signs present on arrival of not being calm at all, were transitioning towards greater calm. Almost invariably, the patient would agree, through the paper bag, that he or she was starting to feel better.
I don't recall having ever lost one of these patients.
Then again at the time, follow-up with our ER patients was not that great. Especially for the Nursing Assistants. Not impossible that one or two may have been having a myocardial infarction or presenting with a pulmonary embolus, only diagnosed subsequently by someone with more medical training (and malpractice insurance) than I had at the time. Most appeared to have recovered quite remarkably, and gave positive feedback for my brown bag intervention.
And I would feel for a little while somewhere between Moses leading the horde across the desert, and Denton Arthur Cooley, MD, heart surgeon, after implanting the first totally artificial heart. Nothng less.
I am not suggesting that these first patients of mine were simply crazy.
Far from that.
It is important to mention that because too often today, some who are assigned to caring for those with "long-term" COVID-19 quickly conclude that such a person is simply crazy. They would agree with their initial triage to "the Psych room."
I am suggesting that the findings were very real, not imagined, and that they were based in physiologic and pathologic principles as valid today as when I had the privilege of experiencing them firsthand 46 years ago.
While many of the "long-term" COVID-19 respondents are measuring peripheral oxygen saturation levels with their pulse ox, to see their oxygen levels, what drives us (and them) to breathe that next breath is much less blood oxygen levels (unless extremely low) than blood carbon dioxide levels. Too high a systemic CO2 level and all the receptors in our spinal cord start screaming in unison: "Breathe!"
And we control that drive with our minute ventilation: the depth and frequency of our breaths over 1 minute.
And as I noted: these particular "long-term" COVID-19 patients weren't measuring that level of CO2. Though they commented on it through their responses by telling about how they were breathing.
And they commented carefully and more completely as their replies and "Other: " choices and explanations for this specific question attest.
------
Hypervigilance for bodily changes is part of this syndrome. There. I've used the word syndrome, and in doing so, suggested that it has several parts. Some obvious. Some not at all obvious.
The hypervigilant person will tend to make others around them nervous.
Such a person perceives a danger. Others around them don't.
Part One: respiratory alkalosis due to hypocapnia.
Hyperventialtion leads to respiratory alkalosis
That means that carbon dioxide (CO2) in the body drops, and can do so rather quickly.
That is called hypocarbia or hypocapnia.
Sometimes patients present hypocapneic. Sometimes due to an underlying illness.
Sometimes we make them so when we overventilate them in an OR or ICU.
What negative effects on the body can hypocapnea have?
An extensive review here will keep us from our journey's end.
But here are some references, and also a summary in a few lines.
- The underlying mechanism of all hypocapnia, is hyperventilation.
- shortness of breath, a frequent complaint
- many pathologies induce respiratory change, so a whole sublist of findings possible from the history and physical examination
- causes cerebral vasoconstriction: dizziness, confusion, seizures, syncope (passing out)
- painful tingling in fingers, toes, sweating of the hands
- tachypnea (increased breathing rate) and tachycardia (heart rate increased)
- in an acute state, noticeable increase in chest wall movements
- in chronic hyperventilation, chest wall movements and rapid breathing may not be apparent
- it leads to reduced Vitamin D levels, which may present as fibromyalgias and tetany
- these lead to the well-known Trouseau's and Chostek's signs of peripheral nerve irritability
- these findings are due to decreased serum calcium, as calcium shifts from serum to be more albumin bound as the blood pH rises (alkalosis).
Many illnesses can be associated with hyperventilation, since essentially every organ of the body can be involved. Respiratory alkalosis is not life-threatening. However, the underlying pathology may be.
Here is a selection of useful references, as promised:
Bench-to-bedside review - Carbon dioxide
Is the Way You Breathe Making You Anxious?
Clinical Review - Panic Disorder
Managing panic disorder in general practice
If Syndromic, Where To Now?
Part Two: Hypophosphatemia
Hyperventiltion causes hypophsphatemia. It does so acutely. It can become a chronic phenomenon.
Many other things do as well. But now that you are an expert on hypocapnia, you need to be or become an expert on hypophosphatemia.
Which of course means, low phosphate levels.
Why are we getting into this? What's the link to "long-term" COVID-19?
Our current hypothesis is that much of that illness is a problem of energetics.
That problem derives from a problem with mitochondria in the cells of these patients.
The viral illness has hijacked their mitochondria for its use. An energy source for its
replication, and that it cannot do without. Creating peripheral damages in its process of making baby viruses is clearly not a concern of this virus.
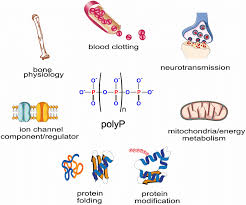
As already presented, mitochondria do many things to keep a body happy.
But they are best known, and correctly so, for being the "powerhouse" of the cell.
They make the only molecule the body uses for its energy needs: ATP.
And to do that, over and over again, mitochondria need ADP and phosphate, among other things.
Phosphate is stored mostly in our bones. Measurements in the blood don't reflect well the total body stores, and instead of being out in the extracellular blood (where it gets measured with a blood sample), much is also intracellular. This being quite consistent with where the mitochondria are found.
It's great that it's intracellular. But if we aren't measuring its level inside the cell, is that level adequate?
How would you know?
Can one develop low levels of phosphate? Yes. Alcoholics do it all the time. When hospitalized, at least 50% are hypophosphatemic.
But for most of us, the diet is thought to be sufficient to provide required phosphorus.
An interesting evolutionary note: most edible and even tasty foods are high in phosphorus.
Most that we don't like frequently have much less phosphorus. Evolution has driven us to find it,
and eat it.
It's sort of an animal thing: Find food (phosphorus). Eat. Avoid being eaten.
It's worked for millions of years, and gotten us to where we are today. Going much beyond that line of hunter-gatherer activity, risks getting us bogged down in myth.
This natural abundance of phosphate is so true that if you go to your local Vitamin Store, and seek to buy some Phosphorus (while perhaps purchasing some Zinc, or VItamin-D, or Selenium, or Magnesium, or Niacinamide), inorganic phosphate is less easy to find. And what is offered is often found in rather small homeopathic doses.
You'll be told, perhaps by the clerk or cashier: "You should get that from a balanced diet."
A "nutritious" diet will provide 1000 to 2000 mg of phosphate daily. 300 mg comes in and 300 mg goes out.
Should be enough.
So here is a sorted list of phosphorus-containing foods, from the US Dept. of Agriculture. Notice Sunflower and other seeds at the top. And here, an image file of phosphate food sources.
So for understandable reasons, the bias is towards thinking that phosphorus is ubiquitous, and so one will never be phosphate depleted, never suffering from a hypophasphatemia.
Well that's:
- Not true
- Here are the effects, and related references below.
- Once reorganized just a bit, hypophosphatemia is a no-holds-barrred attack on the human respiratory system, from nose to red blood cell. (can you now see any links to our "long-term" COVID-19 respondents?) Delivering oxygen to where it's needed, from nose to Electron Transport Chain, needs phosphorus. Get some.
- Basic physiology & pathology, first
-
-
- Normal serum levels of phosphate are 4 to 7 mg/ dL in children, and 3 to 4.5mg/ dL in adults.
- A value less than 2.5 mg/ dL = hypophosphatemia.
- Normally 300 mg pf phosphate is resorbed from bone for use in cellular reactions, and 300 mg deposited each day. This under the influence of parathyroid hormone, Vitamin D and sex hormones.
- Reduced phosphate depends on one of three mecanisms, either: Decreased intake of phosphorus, or Redistribution of phosphorus (movement from extracellular to intracellular for example), or Increased urinary excretion of phosphorus.
- Acute respiratory alkalosis induces hypophosphatemia via changes in cellular pH (less acid).
- Hyperventilation is the most common cause of hypophosphatemia in hospitalized patients.
- Most patients with hypophosphatemia are asymptomatic due to mild levels of abnormality.
- The most common symptom is generalized mild to moderate weakness.
- More severe hypophosphatemia presents with altered mental status, neurological instability, seizures, numbness and reflexive weakness, cardiac manifestations of possible heart failure, muscle pain, muscle weakness.
- Chronic hypophosphatemia presents with bone pain and pathologic fractures. Osteoporosis, rickets, osteomalacia (softening) are due to decreased bone mineralization.
- Central nervous system: metabolic encephalopathy due to ATP depletion manifesting as altered mental ststus, irritability, paresthesias, numbness, seizures, coma.
- Cardiac function: ATP depletion leads to possible systolic heart failure, myocytes become less stable, arrhythmias are possible.
- Decreased diaphragmatic function impacts pulmonary function and leads to hypoventilation.
- Ventilator-dependent patients have a prolonged course and worse outcomes when hypophosphatemia is present.
- Gastrointestinal dysfunction occurs at decreased levels of ATP, with dysphagia (difficulty swallowing), reflux and ileus (lack of intestinal peristalsis and propulsion) possible.
- Generalized muscle weakness occurs.
- Rhabdomyolysis may occur with breakdown of muscle cells, increasing CPK levels and damage to kidneys.
- Hematology: increased RBC rigidity and changes in shape, reduced lifespan (usually 120 days) leading to hemolytic anemias, reduced chemotactic response (movement towards infections) and reduced phagocytosis by white blood cells (engulfing bacteria). Typically, thrombocytopenia (reduced platelet counts and function).
- Symptoms may not be present in mild cases, but abnormalities should be noted and corrected whenever hypophosphatemia is found.
- There are no contraindicatingg reasons for oral replacement of phosphate when indicated.
- Effects of hypophosphatemia are broad and impact nearly every system.
- Medical causes.
-
- Antacids for reflux and other GI symptoms
- Cortocosteroids (stress)
- Diuretics
- Treatment of diabetic ketoacidosis, glucose, insulin
- Salicylate (aspirin) poisoning
- catecholamine (epinephrine and dopamine)
- theophylline, bronchodilators
- estrogens, mestranol
- biphosphonates
- intravenous iron administration
- phenytoin and phenobarbital (cause Vitamin D deficiency and resistence)
- Acetaminophen poisoning
-
-
Some references, as promised:
Medication-induced hypophosphatemia
Effect of hypophosphatemia on the withdrawal from mechanical ventilation
The following study emphasizes 7 effects of hypophosphatemia. But listed first, the reference from which these are drawn:
Hypophosphatemia - an evidence-based approach to its clinical consequences and management
-
- rhabdomyolisis (muscle breakdown)
- hemolysis (breakdown of red blood cells)
- leukocyte dysfunction (seems to be mostly in animals)
- respiratory failure
- impaired myocardial performance
- diabetic ketoacidosis
- perturbed central nervous system
Say. Is this starting to sound like "long-term" COVID-19, or what?
A few more ...
Multiple articles placed together on the effects of hypophosphatemia
Hypophosphatemia-Induced Cardiomyopathy - A Literature Review.
Hypophosphatemia in the Intensive Care Unit - Incidence, Predictors and Management.
Acute hemolytic anemia with rigid RBCs in hypophosphatemia
The degree of hypophosphatemia correlates with the incidence of postoperative complications.
An autocrine ATP release mechanism regulates basal ciliary activity in airway epithelium
Regrouping these effects of hypophosphatemia permits one to see its grave impact on human respiratoy function:
-
- Hyperventilation causes hypophosphatemia
- Hypophosphatemia reduces muscular strength and extent of the diaphragm's excursions
- Ciliary beating to clear secretiong from the airway, is ATP dependent and diminishes with hypophosphatemia. Autocrine mechanisms contribute to ATP release for ciliary beating.
- Calcium levels, acutely influenced by hyperventilation and hypocapnia, regulates phosphorylation and dephosphoryation of ciliary proteins that lead to beating normally. This is markedly reduced by low phosphate levels. This means that secretions build up and aren't cleared.
- Lung epithelial cells are immunologically active and depend on mitochondrial functions that are in turn inorganic phosphate dependent.
- Hypophosphatemia contributes to hemoptysis (blood in the airways) through a direct effect on platelets.
- Hypophosphatemia decreases effectiveness of WBC migration (chemotaxis) and phagocytosis (engulfing foreign particles and bacteria) and contributes to increased risk of pneumonia.
- Hypophosphatemia has mutiple effects on red blood cells:
- It changes their shape and increases their rigidity, leading to hemolytic anemias
- It strikingly reduces red cell ATP
- red cell survival is decreased due to 1 & 2
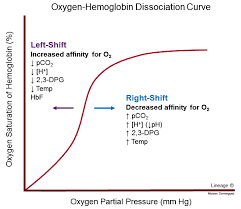
- red cell 2,3 DPG, the substance that determines the position of the oxyhemoglobin dissociation curve, is markedly reduced.
- The oxyhemoglobin dissociation curve is shifted to the left by hypophosphatemia. This means that hemoglobin binds oxygen more tightly, not releasing it in the periphery where needed. The risk of developing tissue hypoxia is increased.
What does this mean? This "shift to the left"?
It means the hemoglobin molecule, a structure that normally carries oxygen molecules around like in a bucket, 4 oxygens at a time, just holds onto it. The red cell takes it out to the periphery (fingers and toes) and instead of dumping off a load of needed oxygen, what does it do?
It carries it back to the heart and lungs. Result? Tissues in the periphery trend towards hypoxia (starved for oxygen).
Say. If you like to measure your oxygen saturation with your pulse oximeter, have you ever noticed kind of pale or blue finegernails much of the time? Well. You don't say.
You'd better just stop shifting your oxyhemoglobin dissociation curve so far to the left.
Got that? Good.
--------
Hypophosphatemia & COVID-19
Part Three: a bit closer to our target
-
-
- In a study from China, ICU patients, mechanically ventillated, who had hypophosphatemia during their treatment for COVID-19, had higher APACHE II scores (higher severity), longer duration of mechanical ventilation, longer ICU stay, and higher mortality levels.
-
Correlation between hypophosphatemia and the severity of Corona Virus Disease 2019 patients.
-
-
- Higher phosphate levels may be associated with better CT scan of lung outcomes in COVID-19; while hypophosphatemia is associated with severe lung injuries.
- Correlation between hypophosphatemia and the severity of Corona Virus Disease 2019 patients (in press) - "There was a positive correlation between lymphocytes and serum phosphorus, and the correlation coefficient was 0.479. Conclusion: hypophosphatemia is related to the severity of COVID-19, and strengthening the monitoring of serum phosphorus level of COVID-19's severe/critical patients and correcting hypophosphatemia in time are of significance to improve the prognosis."
- As the title reads: "Low calcium and low phosphorus could indicate the severity of COVID19 patients, and may be utilized as promising clinical bio-markers for discriminative diagnosis
- "This is an important mechanism to remember in the current COVID-19 pandemic, which has seen health services worldwide placed under strain with very large numbers of patients presenting with respiratory failure."
-
Phosphate metabolism and respiratory alkalosis - a forgotten lesson in COVID-19.
-
-
- "Available data show that phosphate and Mg are deficient in COVID39 19 with phosphate showing a remarkable correlation with its severity. We thus argue that COVID-19 patients should be monitored and treated for phosphate and Mg deficiencies, ideally already in the early phases of infection. Supplementation of phosphate and Mg combined with vitamin D could also be implemented as a preventative strategy in populations at risk. "
-
-
-
- "Hypophosphatemia has been observed to correlate with lymphocyte count and severity of COVID-19. In a small study in China of 20 critically ill patients, hypophosphatemia was observed in 50% of the severe cases. The stress burden of the viral infection and gastrointestinal losses due to impairment of the mucosal integrity could contribute to hypophosphatemia. Maintenance of the serum phosphorus level within the normal range may improve respiratory support and promote the function of the immune system."
-
Pathogenesis, clinical manifestations and complications of COVID-19.
-
-
- If one to three inorganic phosphates in a row (on AMP, through ADP, to ATP) is good, perhaps a whole string is even better. Polyphosphate, produced by platelets, blocks spike protein attachment to ACE2 receptors. Isn't that neat ...
-
"So What Is The Syndrome Here ?"
Here are the components summarized:
-
-
- The questionnaire (September-October, 2020) responses teach that breathing is abnormal in this sample of patients suffering "long-term" COVID-19.
- The reported breathing patterns strongly suggest periods of hyperventilation during at least some part of this illness.
- Whether at a given time a patient presents initially with anxiety, or with hypocarbia and hyperventilation is totally unimportant. Physical and emotional manifestations of the illness of hypophosphatemia are clearly present, our respondents told us so. This must be so if the rest of the explanation is to make sense.
- The resulting hypocarbia or hypocapnea has its various known effects, and these are well represented in the physiology and Medical literature from long ago - the patients' lists of symptoms and frequencies of each, speak to these known effects.
- One effect of this illness (COVID-19) and through several modalities, is to reduce body phosphate stores, but also measured blood levels. - the patients' lists of symptoms speak to this as well.
-
-
- A very important jump beyond what might be the usual therapeutic reflex at this point, must take place.
- That reflex, placed here on a back burner, could be stated as "low phosphorus, give phosphorus."
We would predict that that response, while acceptable and likely safe in almost all circumstances one can imagine, and might even help many..., may not be effective for most. Here's why:
We'd like to see normal phosphorus levels because the mitochondria would normally like that as well. But ...
Fix first, what must be fixed first.
Otherwise, fixing problem number two first, before addressing problem number one, might not make any difference: might lack effectiveness.
Mitochondria:
They're the "powerhouse" charged with cranking out the ATP needed by the cell. They need, among other things, a recycled ADP, and an inorganic phosphate to get the job done: over and over again. The other things needed: Magnesium, Copper, NAD+, FAD+, protons, electrons, a membrane to maintain a proton gradient, and more ...
all of that mitochondrial machine will fall sadly short of the production quotas. Why? Because too many ATPSynthase-coupled enzyme systems have taken a hit. They have been damaged or hijacked or both by the virus in its march through the body with only one goal: making viral babies. After 6.5 months or more, these "powerhouses" are all pooped out. They haven't gotten over that attack. That sounds like a mitochondrial disease.
So until that gets repaired, until all the cytochrome 'c' oxidases get some energy from elsewhere, that terminal donation of electrons in the Electron Transport Chain may just putter along.
May in fact putter along for 6 or 7 months or more, while the owner of all those mitichondria and phosphates just putters along, with marked fatigue, "brain fog," confusion, muscle aches and pains, hair falling out, reflux esophagitis, funny smells and tastes, and shortness of breath. And oh yes as well, anxiety, frustration, depression, and occasional suicidal ideation. Preferring to ignore all of that, is to ignore completely this questionnaire presented on this site and especially, the responses obtained. You decide.
We picked on Inorganic Phosphorus. We could have chosen Magesium (Mg2+).
The presentations here should not start to resemble a textbook in length. Some already have.
But yes, respiratory alkalosis impacts magnesium levels as well.
Important? Yes.
- Mitochondria are intracellular magnesium stores.
- Magnesium has a clear relationship to many diseases including obesity, type-2 diabetes, cancer, and neurological diseases.
- Magnesium is an important second messenger in our immune system.
- It is a multi-terget metabolic regulator.
- Dysregulation of mitochondrial Mg2+ homeostasis affects cellular energy maintenance and viability.
To avoid branching off too far, we place here some references on the importance of magnesium in exactly the situation where "long-term" COVID-19 respondents find themselves.
But again, if the machinery is down, just feeding it more magnesium may have a less than anticipated and hoped for result.
Magnesium and Other Biometals in Oxidative Medicine and Redox Biology.
Mitochondrial Mg2+ homeostasis decides cellular energy metabolism and vulnerability to stress.
-------
Sound like anyone we know?
So to those who still find themselves thinking that all those individuals presenting with "long-term" COVID-19 are perhaps just a little crazy...,
I would respond: "with everything that their bodies are going through, they should be even crazier."
They are looking for a way to get back to doing; to living a life; to moving around; to being done with this.
But until those cellular organelles at the power plant get fixed, they may still have a long wait for a probable gradual recovery back to sought after pre-illness levels.
Eventually, and perhaps simultaneous with eating sunflower seeds throughout the day to replenish low phosphate (see the list above for other choices), we've got to shine a light on this.
Keeping a brown paper bag handy is also a good idea. That's not a disguised insult.
It can be very handy and they're cheap. I buy 125 from here for €7.20. Buy 1000 if you like, and share with friends.
Getting up tight? Breathing a littlie weird? Get the bag. Seal it over nose and mouth. Breathe into it like that for 10 minutes. Chill.
You're saving your phosphate, and shifting your oxyhemoglobin dissociation curve right back to where it belongs. You'll be delivering more oxygen to your bluish fingernails.
For some it might prove to be the best medicine proposed so far.
Here's the Energetics behind the responses to the Questionnaire >>>>>>
<<<<<<< Home